Sepsis Interdisciplinary Research Center (SIRC) at SUNY Upstate Medical University
The term sepsis describes the overwhelming host response to infection. Sepsis is a major and very challenging medical problem, annually impacting 1.7 M Americans and causing 270,000 deaths. Sepsis is the leading cause of death in hospital. The mortality rate of sepsis remains high although huge efforts have been invested in sepsis research and treatments. Due to the complexity of sepsis, none of the experimental therapeutics developed over the last decades have proven to be effective. During sepsis, the combination of severe infection and host response to infection causes systemic inflammation and tissue damage. The release of damage-associated and pathogen-associated molecular pattern molecules (DAMPs and PAMPs) activate the innate immune system by interacting with pattern recognition receptors. Therefore, tissue damage during some critical illness, e.g. trauma, burn, acute lung injury (ALI), cirrhosis, and pancreatitis can result in sepsis via a common pathophysiological pathway, i.e. systemic inflammatory response syndrome (SIRS) (Scheme 1), which further leads to septic shock, multiple organ failure and potentially death.
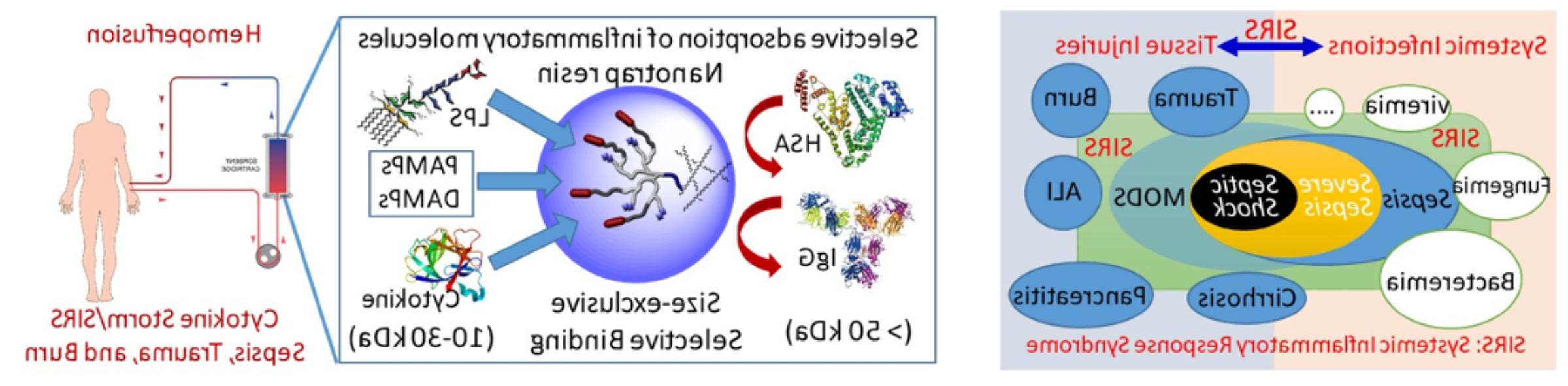
Scheme 1. Illustration of sepsis induced by both infections and traumatic tissue injury through a common pathophysiological process, e.g. systemic inflammatory response syndrome (SIRS). A novel nanotrap hemoperfusion approach has been developed in Dr. Juntao Luo’s Lab at SUNY Upstate Medical University to selectively scavenge a broad range of septic triggers, mediators and signalling molecules to attenuate hyperinflammation in sepsis and critical illness patients.
Dr. Juntao Luo at SUNY Upstate Medical University has developed an innovative nanotrap technology to attenuate the host’s inflammatory response to infection by scavenging a broad range of PAMPs and DAMPs. This novel nanotrap technology can be designed to target specific pro- or anti-inflammatory signaling molecules, selectively, therefore, precisely controlling immune responses. Nanotrap technology can be applied systemically (nanoparticles), or locally at the site of infection (nanogel and hydrogel), or extracorporeally as hemoperfusion cartridges at different stages of infection/sepsis to modulate the host’s immune response. This novel technology promises to make a breakthrough and fulfill the unmet clinical need for sepsis treatments. Through collaboration, these nanotrap approaches are being evaluated in clinically applicable large animal models to demonstrate the evidence-based efficacy for sepsis treatment at both molecular and systemic levels for clinical translation.
Sepsis Research at Upstate
Sepsis research at Upstate has a long history, focusing on preclinical and translational research aimed at developing and evaluating therapeutic approaches for sepsis treatment in highly clinically-relevant porcine sepsis models. In response to the National initiative in solving sepsis through driving innovation and accelerating transformative technologies, Dr. Robert Cooney, MD, Professor and Chair of Surgery, and Dr. Juntao Luo, PhD, Associate professor of Pharmacology, have co-founded the Sepsis Interdisciplinary Research Center (SIRC) and serve as co-directors to modulate research collaborations and grant applications in translational sepsis research.
SIRC is a highly collaborative and integrative research group with synergistic and multidisciplinary expertise from therapeutic development, molecular biology, immunology, pathophysiology and clinical care. Eight laboratories in the Department of Pharmacology and the Department of Surgery are actively conducting research in sepsis, trauma, wound healing, pulmonary and hematological diseases, funded by multiple active federal grants, including four NIH R01 grants, and R21, NSF, and DoD awards.
